Case Vignette
A 46-year-old male, non-smoker, hypertensive with controlled BPs and known case of Glottic Squamous Cell Carcinoma stage IV with history of 35 sessions of radiotherapy and tracheostomy, is admitted for one week history of progressive difficulty of breathing with no associated fever. Physical examination showed a fully conscious and oriented patient with vitals of BP 120-130/60-70 HR 100-110, there was no note of jugular venous distension. Patient was noted to have decreased breath sounds on bilateral lower lung fields and muffled heart sounds, abdominal PE was unremarkable and the patient was noted to have full pulses and warm extremities without edema.
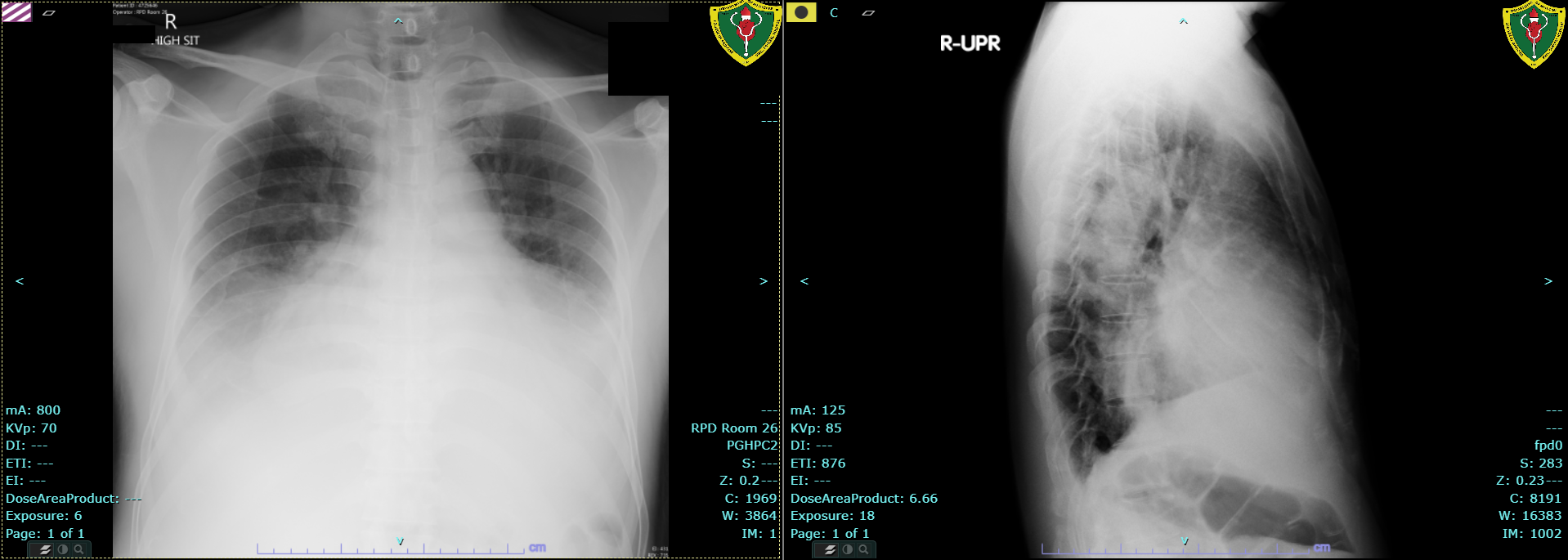
Workup of the patient included a CBC with Leukocytosis of 6500 with neutrophilic predominance of 83%, hemoglobin was 128 g/L platelets were at 350,000. Chemistry revealed an elevated creatinine of 124 umol/L (eGFR 58.99) with normal AST, ALT and rest of electrolytes. Chest radiography showed multi-chamber cardiomegaly and lobar pneumonia, pericardial effusion was entertained on this xray. The patient was treated for pneumonia with appropriate antibiotics.
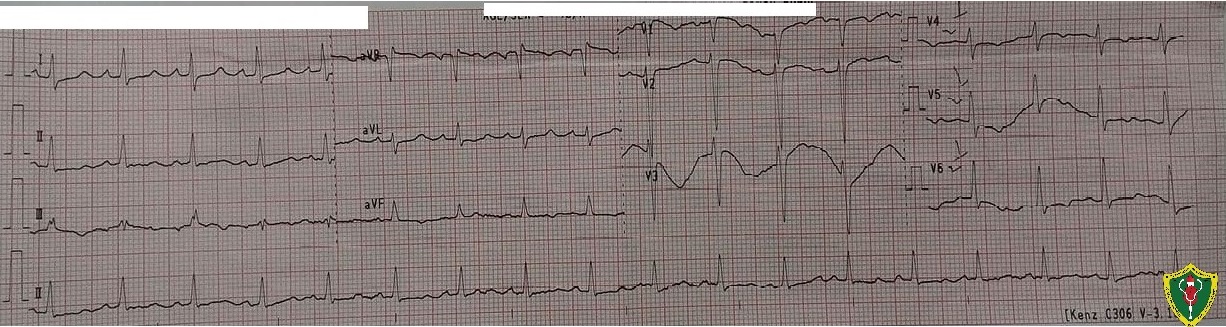
12L Electrocardiogram showed regular sinus rhythm, with a rate of 107 bpm, normal axis and non-specific ST-T wave changes. The actual QT interval was noted to be 0.32 msec, with a corrected value of 0.427 msec, denoting a normal QT interval
Chest radiography showed the following image:
The patient would develop hypotension during his course and associated decrease in sensorium, but this would improve with pressor support with Norepinephrine and escalation of antibiotics. Serial Troponins were taken and revealed no significant increasing trend. It was found during the course that the patient had poor compliance to Thyroid replacement therapy. TSH was found markedly elevated at 48.09 uIU/ml.
Surveillance point-of-care 2D Echocardiography done still showed moderate-to-large pericardial effusion not in tamponade. A follow up full 2D Echocardiography was done showing a moderate pericardial effusion with invagination of the left atrium during early diastole. The left ventricle was noted to have global hypokinesia with an ejection fraction of 22%
|
|
In this case drainage of the pericardial effusion is appropriate because of the underlying malignancy.2 The causes of the pericardial effusion in this case could be severe hypothyroidism versus a malignant cause such pericardial metastases from a primary malignancy. Hence, drainage here was done to resolve persistent effusion which may progress to tamponade, as well as, to investigate the etiology of the effusion. The patient underwent pericardial drainage which he tolerated well. Work up of the pericardial effusion did not reveal any malignant cells.
References:
- http://www.acc.org/education-and-meetings/patient-case-quizzes/2018/02/13/07/12/should-a-large-pericardial-effusion-be-drained
- Adlery Y., Charron, P., Imazio, M., et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the task force for the diagnosis and management of pericardial disease for the European Society of Cardiology (ESC) endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS) Eur Heart J. 2015:36:2921-64.
